-
A friendly and supportive community, register today. Our forums use a separate account system.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Clinics CB1 Medical
- Thread starter GrownHealth
- Start date
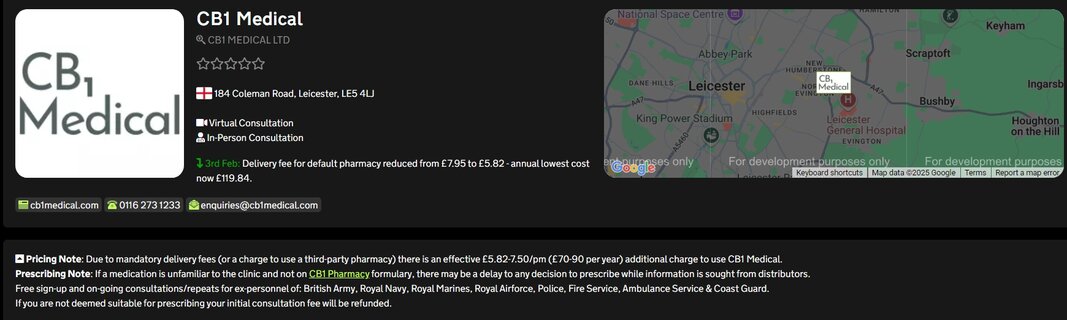
As you suggested, free for personnel of various national services or armed forces veterans - otherwise £50 per year. By far the cheapest clinic, with generally favourable reviews as far as we've seen.
You can use any pharmacy at CB1 Medical, though they also have a public formulary for their own pharmacy posted here:
You can use any pharmacy at CB1 Medical, though they also have a public formulary for their own pharmacy posted here:
Cheers, I get it now, I was thinking it was £50 for personnel of various national services and armed forces veterans and couldn't find prices for others, making me think it was exclusive. Going to look into this , the cost over a year for a new patient not just the £50 but the oils and flower costs with any Grow Access Project or T21 discount if applicable for someone, must admit looks promising compared to some others at first glance.As you suggested, free for personnel of various national services or armed forces veterans - otherwise £50 per year. By far the cheapest clinic, with generally favourable reviews as far as we've seen.
You can use any pharmacy at CB1 Medical, though they also have a public formulary for their own pharmacy posted here:

The CB1 Formulary
docs.google.com
BudWarrior
Filling Out
The idea of less frequent appointments matters. Makes CB1 Medical attractive, if also true like Mamedica®.
Great feeling having no consultation required for bout another nine months for me, difference is this person would probably need guidance with the oils and I'd imagine the need for THC/high CBD oil so may need more consultations as they find out what works for them oilwise, so would not like the outlay for an access scheme that becomes value in the second year encase the benefits of MC are not significant enough also these oils I suspect they would need tend to be really dear. With me the need for guidance isn't as essential as I've treated my mental health and kept it check myself with cannabis for years.I just needed access to the tools so to speak.The idea of less frequent appointments matters. Makes CB1 Medical attractive, if also true like Mamedica®.
BudWarrior
Filling Out
difference is this person would probably need guidance with the oils and I'd imagine the need for THC/highcbd oil so may need more consultations as they find out what works for them oilwise
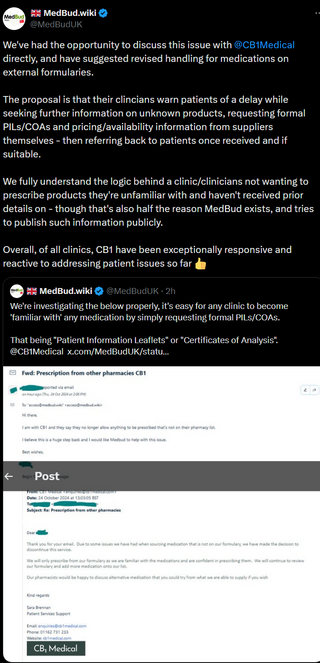
We've learnt that CB1 Medical are introducing a £7.50 postage fee for prescriptions sent to external pharmacies.
While offering either entirely free patient care, or £50 per year, the clinic loses money on every single prescription sent elsewhere from the cost of Royal Mail Special Delivery <1pm envelopes.
We have already fed back that we're not sure on the regulatory compliance overall, as it does financially bias/incentivise prescriptions sent to their own pharmacy.
Other lower cost postage methods for external prescriptions are being evaluated, and could reduce this fee moving forward.
We're also aware Newgrove will cover/deduct the £7.50 fee from the total of any prescription invoice sent to them.
It's standard practice for some pharmacies to supply free pre-paid envelopes to clinicians - we're hoping some pharmacies may do this for CB1 Medical prescribers, where fees can then be removed again for patients
We'll update as things develop.
While offering either entirely free patient care, or £50 per year, the clinic loses money on every single prescription sent elsewhere from the cost of Royal Mail Special Delivery <1pm envelopes.
We have already fed back that we're not sure on the regulatory compliance overall, as it does financially bias/incentivise prescriptions sent to their own pharmacy.
Other lower cost postage methods for external prescriptions are being evaluated, and could reduce this fee moving forward.
We're also aware Newgrove will cover/deduct the £7.50 fee from the total of any prescription invoice sent to them.
It's standard practice for some pharmacies to supply free pre-paid envelopes to clinicians - we're hoping some pharmacies may do this for CB1 Medical prescribers, where fees can then be removed again for patients
We'll update as things develop.
Rimmerworld
Filling Out
- Messages
- 420
- Likes/Reactions
- 631
- Clinic
- 🏴 Mamedica®
They will send scripts to any external pharmacy, there's just a £10 fee similar to the above.and wont send any scripts to external pharmacys
Again, I really don't think this should be happening either.Mamedica® list thier own strains alpuabetically with m above a lol
Whos regulating or enforcing that? Theres no one.

Care Quality Commission branded “not fit for purpose” as review finds “significant failings”
Health secretary Wes Streeting has said that the CQC (CQC) is “not fit for purpose,” after an interim review of the regulator of health and social care in England found significant failings, including a lack of clinical expertise among inspectors, inconsistent assessments...
Rimmerworld
Filling Out
- Messages
- 420
- Likes/Reactions
- 631
- Clinic
- 🏴 Mamedica®
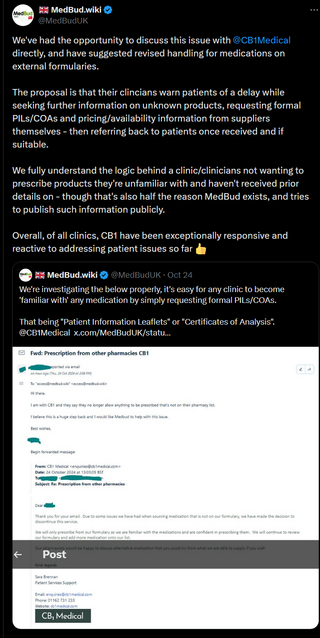
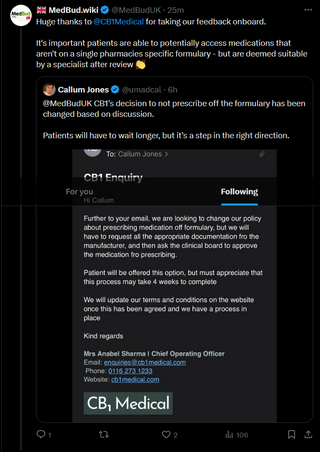
They will send scripts to any external pharmacy, there's just a £10 fee similar to the above.
Again, I really don't think this should be happening either.

Care Quality Commission branded “not fit for purpose” as review finds “significant failings”
Health secretary Wes Streeting has said that the CQC (CQC) is “not fit for purpose,” after an interim review of the regulator of health and social care in England found significant failings, including a lack of clinical expertise among inspectors, inconsistent assessments...www.bmj.com
The Mamedica® situation always confused me thanks for clarifying. CQC havent did anything to mamedica so no wonder CB1 Medical started doing it. If you dont enforce the rules then people will assume they arent rules anymore.
Indeed, and 6+ months ago we warned that this would happen. The problem is the toothlessness of clinic/pharmacy regulators when dealing with situations like this.If you dont enforce the rules then people will assume they arent rules anymore.
From the commercial side and CB1 Medical's perspective, I get their need to charge - but I also personally don't believe any clinic should be charging any more or less for accessing particular pharmacies. Neutrality and impartiality are incredibly important in healthcare/medicine.
There's been talk for a while of some special governmental body/committee devoted to medical cannabis, we'll see what happens. APPG for medical cannabis should start back up before long too - and that's where we could see real change instigated.
My wife just signed up with CB1 Medical , straight forward and £50/Year ,sweet as. Just less than 3 weeks for appointment I suppose this is to be expected with the offer they have.
Onwards and upwards.
Onwards and upwards.
BudWarrior
Filling Out
To be fair to them, I worry slightly about their business model, if too many prescriptions are fulfilled external to their formulary.
When clinic costs are low, squaring the circle of a sustainable business is possible when it's all dispensed in house. When it's dispensed externally instead, they don't get that revenue cut. So their business is less lubricated.
They likely can't charge for external prescriptions only because they are external, for basic regulatory reasons. Independence / freedom of prescribing and dispensing maintains patient choice). So they can't go that way.... In pure commercial law terms, it would also be an anticompetitive restrictive trading practice.
Maybe the sums can be made to add up - I don't have their books. But I do worry about whether these fast growing young businesses stay liquid. It's a classic that businesses make enough revenue on paper, but cashflows crunch. Let alone recruitment challenges or just making enough revenue full stop.
@Muiredach, if my superficial worry is real. A central product DB like MedBud and its inventory data per SKU could be a solution for industry stability. An industry utility. Compatible with the current vision. And not locked into commercial operations, which others' equivalent solutions would be.
If stock data is up to date, then just on time wholesaling and drop shipping is made easier for pharmacies. Which would matter, cos it would avoid any need for dubious external-only prescription charges. Instead, pharmacies could instead confidently list xyz that they don't actually stock, but with a little markup that compensates for lost revenue when it's fulfilled by another pharmacy.
Some people might wonder what I'm on about... But CB1 Medical offers super lean pricing, and the clinics have to be durable. The same would also facilitate lower pricing outfits, who aren't subsidising clinic consultation for their patients.
If they aren't durable, we'll go in a spiral of Jorja Emerson Centre type problems or worse. And if that keeps happening, there will be serious and negative policy attention by government or regulators. Which might be a negatively prejudicial.
When clinic costs are low, squaring the circle of a sustainable business is possible when it's all dispensed in house. When it's dispensed externally instead, they don't get that revenue cut. So their business is less lubricated.
They likely can't charge for external prescriptions only because they are external, for basic regulatory reasons. Independence / freedom of prescribing and dispensing maintains patient choice). So they can't go that way.... In pure commercial law terms, it would also be an anticompetitive restrictive trading practice.
Maybe the sums can be made to add up - I don't have their books. But I do worry about whether these fast growing young businesses stay liquid. It's a classic that businesses make enough revenue on paper, but cashflows crunch. Let alone recruitment challenges or just making enough revenue full stop.
@Muiredach, if my superficial worry is real. A central product DB like MedBud and its inventory data per SKU could be a solution for industry stability. An industry utility. Compatible with the current vision. And not locked into commercial operations, which others' equivalent solutions would be.
If stock data is up to date, then just on time wholesaling and drop shipping is made easier for pharmacies. Which would matter, cos it would avoid any need for dubious external-only prescription charges. Instead, pharmacies could instead confidently list xyz that they don't actually stock, but with a little markup that compensates for lost revenue when it's fulfilled by another pharmacy.
Some people might wonder what I'm on about... But CB1 Medical offers super lean pricing, and the clinics have to be durable. The same would also facilitate lower pricing outfits, who aren't subsidising clinic consultation for their patients.
If they aren't durable, we'll go in a spiral of Jorja Emerson Centre type problems or worse. And if that keeps happening, there will be serious and negative policy attention by government or regulators. Which might be a negatively prejudicial.
Last edited:
This is something that did occur to us and the hope is that prescriptions can be satisfied inhouse without too much of a compromise ,as I feel when signing up in this instance your sort of buying into their way . Also like the way it seems more closely aligned to the NHS , I may be wrong ,but the feedback to the NHS I would of thought that only good would come of this eventually.To be fair to them, I worry slightly about their business model, if too many prescriptions are fulfilled external to their formulary.
When clinic costs are low, squaring the circle of a sustainable business is possible when it's all dispensed in house. When it's dispensed externally instead, they don't get that revenue cut. So their business is less lubricated.
BudWarrior
Filling Out
The NHS side of it makes applying easier, but is less about alignment, and more about API/geek access to commercial medical record systems like EMIS.
That's how commercial apps for patients get access. Apps like the Patient Access and even the eventual English NHS app that did come along.
(But my understanding is that's all API access, cached temporarily, not stored. Hence the Palantir discussions in the media, which will not just be about signing the contract, but also to allow storage/copying to facilitate analytics. Personally, I'd trust that Palantir as far as I could throw Omnicorp from RoboCop, with lots of inside reasons for saying that).
That's how commercial apps for patients get access. Apps like the Patient Access and even the eventual English NHS app that did come along.
(But my understanding is that's all API access, cached temporarily, not stored. Hence the Palantir discussions in the media, which will not just be about signing the contract, but also to allow storage/copying to facilitate analytics. Personally, I'd trust that Palantir as far as I could throw Omnicorp from RoboCop, with lots of inside reasons for saying that).
Soon as you mentioned Palantir I thought , I've heard of them ,checked it an yes it came flooding back ,highly trustworthy set of people/technologies 


More good news .
Rainbone
Filling Out
- Messages
- 290
- Likes/Reactions
- 704
- Clinic
- 🏴 CB1 Medical
Just installed the app. Tried filling everything out it said it is missing but it's gonna take a lot of getting used too for me personally. The request system was so simple before.
trying to put my request in and it is giving me a THC limit reached when trying to add to the request more than one item above 20% THC and I'm well within this months prescriptions allowance.
I really hope I have just done something wrong or there's just a few glitches in the system they can fix soon. I cant wrap my head around it at the moment. Caught myself a lovely cough few days ago so my brain is too fuzzy to focus on dealing with the app at the moment.
trying to put my request in and it is giving me a THC limit reached when trying to add to the request more than one item above 20% THC and I'm well within this months prescriptions allowance.
I really hope I have just done something wrong or there's just a few glitches in the system they can fix soon. I cant wrap my head around it at the moment. Caught myself a lovely cough few days ago so my brain is too fuzzy to focus on dealing with the app at the moment.
Similar Discussions (Automatically Generated)
- Replies
- 9
- Views
- 316